Eligibility Verification
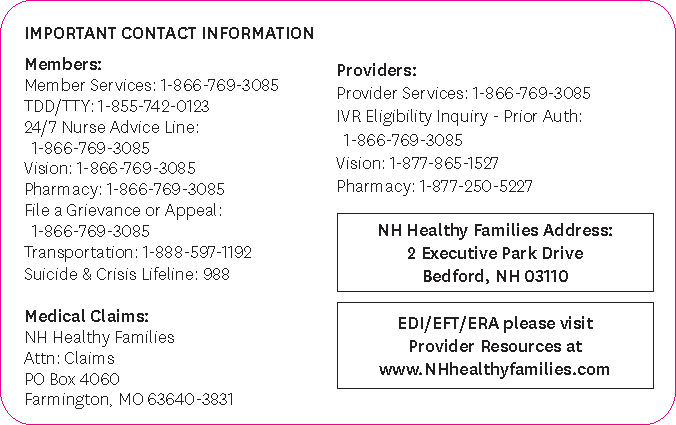
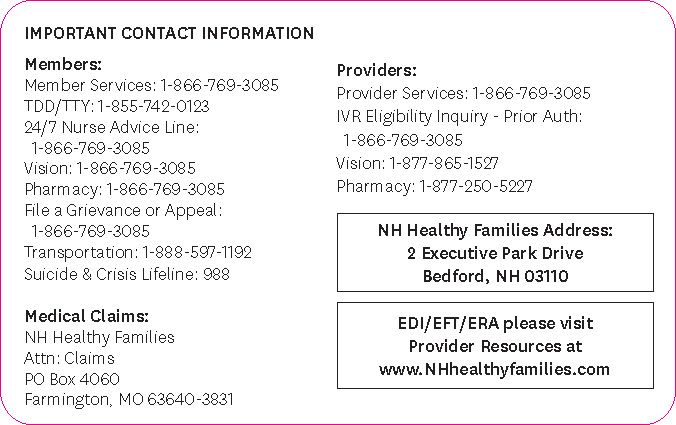
Providers are responsible for verifying eligibility every time a member is seen in the office. PCPs should also verify that a member is assigned to them.
Eligibility can be verified through:
Logging on to the NH Healthy Families secure provider portal
(note: Providers must be registered to access secure portal content)
- View Member Overview
- Look at Eligibility History.
- Under product name:
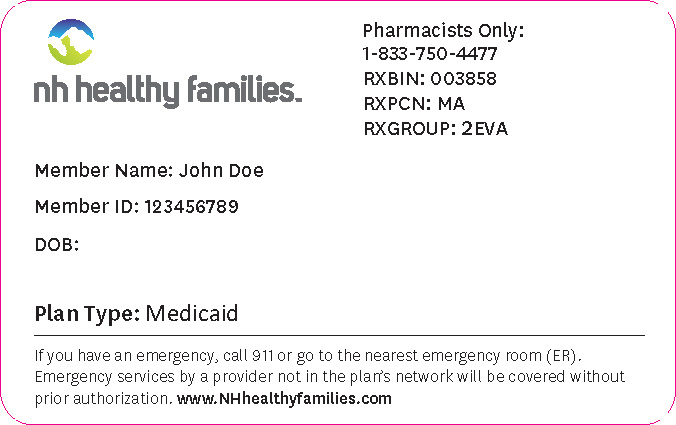
- "Managed Care Program" represents a NH Medicaid client.
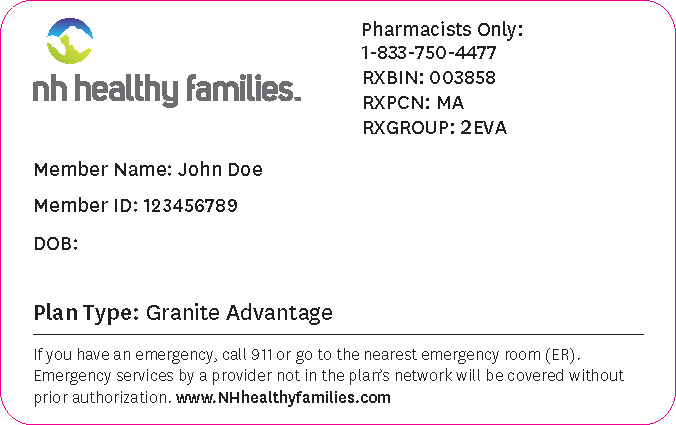
- "Granite Advantage" represents the Granite Advantage Health Care Program* enrollee.
Calling the NH Healthy Families Online IVR system by calling toll free 1-866-769-3085.